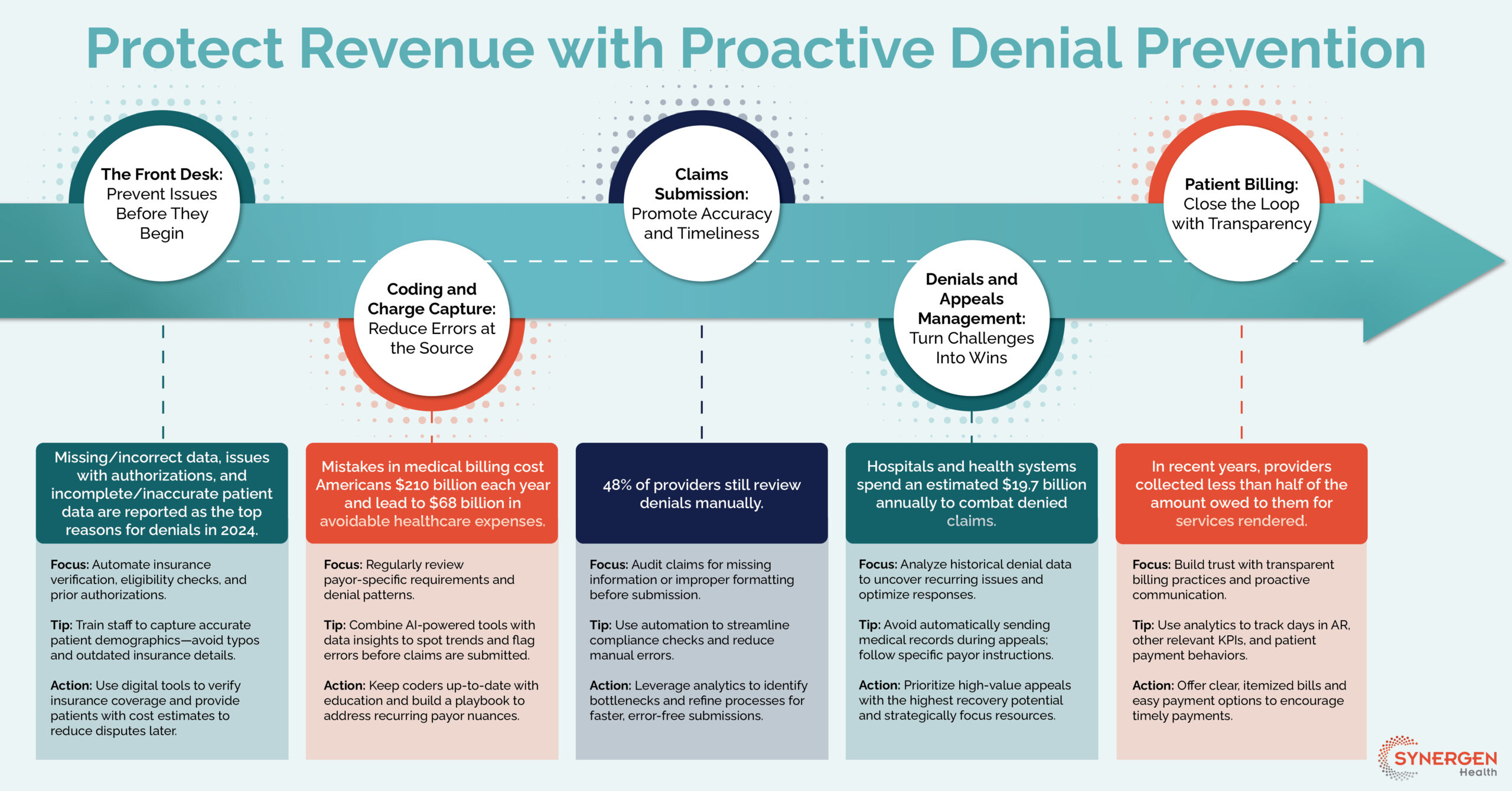
The Front Desk
Prevent Issues Before They Begin
- Focus: Automate insurance verification, eligibility checks, and prior authorizations.
- Tip: Train staff to capture accurate patient demographics—avoid typos and outdated insurance details.
- Action: Use digital tools to verify insurance coverage and provide patients with cost estimates to reduce disputes later.
Missing/incorrect data, issues with authorizations, and incomplete/inaccurate patient data are reported as the top reasons for denials in 2024.
Coding and Charge Capture
Reduce Errors at the Source
- Focus: Regularly review payor-specific requirements and denial patterns.
- Tip: Combine AI-powered tools with data insights to spot trends and flag errors before claims are submitted.
- Action: Keep coders up-to-date with education and build a playbook to address recurring payor nuances.
Mistakes in medical billing cost Americans $210 billion each year and lead to $68 billion in avoidable healthcare expenses.
Claims Submission
Promote Accuracy and Timeliness
- Focus: Audit claims for missing information or improper formatting before submission.
- Tip: Use automation to streamline compliance checks and reduce manual errors.
- Action: Leverage analytics to identify bottlenecks and refine processes for faster, error-free submissions.
Denials and Appeals Management
Turn Challenges Into Wins
- Focus: Analyze historical denial data to uncover recurring issues and optimize responses.
- Tip: Avoid automatically sending medical records during appeals; follow specific payor instructions.
- Action: Prioritize high-value appeals with the highest recovery potential and strategically focus resources.
Hospitals and health systems spend an estimated $19.7 billion annually to combat denied claims.
Patient Billing
Close the Loop with Transparency
- Focus: Build trust with transparent billing practices and proactive communication.
- Tip: Use analytics to track days in AR, other relevant KPIs, and patient payment behaviors.
- Action: Offer clear, itemized bills and easy payment options to encourage timely payments.