As healthcare organizations face increasing financial pressures, managing cost-to-collect is critical for maintaining operational efficacy and ensuring quality patient care.
The “cost-to-collect” in healthcare refers to the expenses associated with billing and collecting payments for medical services from patients, insurance companies, or other payers. This financial metric is crucial for healthcare organizations as it indicates the efficiency and effectiveness of their revenue cycle management processes. Specifically, it measures how much it costs your organization to collect earned revenue.
Calculation:
Total cost of revenue cycle operations*
Total revenue collected during the same period
= Cost-to-collect
*including staff salaries, technology and infrastructure expenses related to billing and collections, and other related overheads
A high cost-to-collect can substantially drain resources and lead to inefficiencies affecting your entire organization. Adopting strategic measures that streamline the revenue cycle processes and reduce these costs is crucial.
These strategies focus on key areas such as minimizing the days in accounts receivable (A/R), enhancing billing accuracy, preventing claim denials, and leveraging advanced technologies. Each strategy aims to reduce the financial burden of billing and collections and improve cash flow to allow healthcare providers to reinvest in patient care and service improvements.
1. Reduce Days in A/R
Typically, the ideal range of days in accounts receivable (A/R) is about 30 to 50 days. Anything more than 90 days indicates potential inefficiencies in the billing process, delayed payments, or issues with claims management—all of which increase the cost of revenue collection.
When healthcare organizations manage to decrease their days in A/R, they effectively reduce the time lag between providing services and receiving payment for them. This reduction is directly linked to lowering the cost-to-collect because it decreases the need for extensive follow-ups and complex collection processes.
Each day that a bill remains unpaid increases the probability of non-collection and necessitates additional administrative effort—resulting in higher labor costs and potentially more write-offs of uncollectible debts.
To effectively reduce the days in A/R and lower the cost-to-collect, healthcare organizations can implement several key strategies:
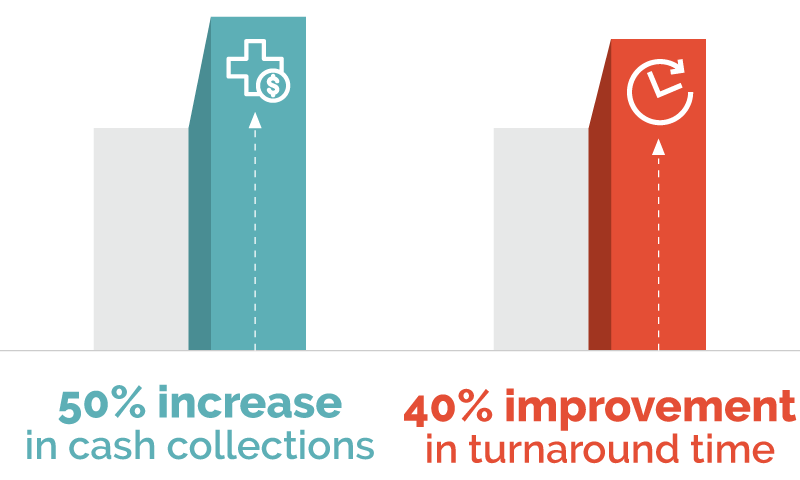
- Improving billing processes: Using technology or specialized expertise to enhance accuracy while increasing the speed of your coding and billing creates enhanced cash flow (we’ve seen a 50% increase in cash collections and a 40% improvement in turnaround time) and prevents denials.
- Rigorous follow-up processes: Automated systems can track claim statuses and flag those that have been pending for too long or denied to enable timely corrective actions. These systems can prioritize follow-up activities based on the age of the A/R and the value of claims, ensuring that staff focus on the most impactful cases first.
- Engaging patients early in the billing cycle: Transparent communication about costs and billing procedures at the point of service can increase the likelihood of on-time payments. Providing multiple convenient payment options and implementing pre-service payment policies for non-emergency care can expedite receivables.
2. Prevent Denied Claims
Denied claims can wreak havoc on every aspect of your revenue cycle, including your cost-to-collect.
Why? Reworking denied claims is a major administrative lift that severely impedes cash flow. Once you receive a denial, staff members must make additional efforts to review, correct, and resubmit the claim, consuming time and resources that could have been directed toward processing new claims or other revenue-enhancing activities.
For example, pursuing denials across all payer types cost providers $20 billion in 2022. The same report states that it took an average of three rounds of interviews with insurers, ranging from 45 to 60 days, to resolve the denial and gain payment. Additionally, providers couldn’t recoup costs for up to six months after delivering care.
To combat denied claims challenges and reduce cost-to-collect, you can adopt several strategic approaches:
- Enhancing pre-claim submission processes: Implementing advanced software that automatically checks for common coding errors and verifies patient eligibility before claims are submitted can drastically reduce denials. This step is crucial in ensuring that claims meet all payer-specific requirements.
- Leveraging AI-driven denials management technology: AI-driven denial management technology can predict and prevent potential denials through pattern recognition and preemptive corrections. Additionally, it can automate the resolution process for already denied claims and streamline resubmission.
- Implementing continuous feedback loops: Establishing a system that continuously collects and analyzes feedback from the claims processing workflow can identify inefficiencies and areas for improvement. This ongoing review helps adapt processes to changing regulations and payer policies, further reducing the risk of denials.
3. Leverage Automation
Automation technologies such as robotic process automation (RPA), machine learning (ML), and artificial intelligence (AI) have the power to significantly reduce the cost-to-collect by streamlining operations, minimizing manual errors, and enhancing efficiency, contributing to substantial cost savings.
Robotic Process Automation (RPA): RPA tools are adept at handling repetitive, rule-based tasks that are prevalent in patient registration, insurance verification, billing, and claims processing. RPA can automate tasks such as data entry, claims status checks, and patient scheduling, which reduces the need for manual labor and ensures they submit claims correctly the first time, reducing the number of denials and the need for costly rework.
Machine Learning (ML): ML algorithms excel at analyzing large datasets to identify patterns and predict outcomes. In the context of healthcare billing, ML can be used to predict which claims are likely to be denied based on historical data. This allows healthcare providers to preemptively address issues in claims before submission, thereby increasing the likelihood of first-pass claim acceptance. ML can also optimize the billing cycle by identifying the most efficient ways to allocate resources, further reducing administrative costs.
Artificial Intelligence (AI): AI extends the capabilities of ML by not only predicting outcomes but also making intelligent decisions based on real-time data. AI can automate complex decision-making processes involved in personalized billing experiences. This reduces the strain on human resources and enhances patient satisfaction, which indirectly contributes to the financial health of the institution by promoting timely payments and patient loyalty.
Strategies for automating processes to reduce costs include:
- Enhanced billing and coding automation: Traditional methods require coders to manually enter service codes, a process susceptible to errors and inconsistencies. Automated coding systems, however, can extract relevant information from electronic health records (EHRs) and apply the appropriate billing codes accurately. This not only speeds up the billing process but also ensures compliance with current medical coding standards, reducing the risk of audits and compliance issues.
- Automate claim tracking and follow-ups: Instead of manual tracking and managing of unpaid claims, automated systems can monitor payment statuses and alert staff about delays or denials. This allows for timely interventions and reduces the duration of the accounts receivable cycle. Automated reminders to patients about upcoming or overdue payments can also increase the rate of on-time payments and improve cash flow.
- Real-time analytics and reporting: With access to comprehensive data analytics, healthcare providers can identify trends, assess the performance of their revenue cycle, and make informed decisions to further reduce costs and enhance efficiency. For example, analytics can reveal common causes of denials or underpayments, allowing organizations to proactively adjust their processes and prevent future financial losses.

Automation technologies such as robotic process automation (RPA), machine learning (ML), and artificial intelligence (AI) have the power to significantly reduce the cost-to-collect.
4. Enhance Patient Communications
Effective communication is not merely a courtesy but a crucial component of the billing and payment process.
Failure to clearly and promptly convey information to patients about billing, insurance benefits, and payment responsibilities leads to misunderstandings, delayed payments, and increased administrative burdens.
Inadequate communication often makes patients unaware or confused about their financial obligations. When patients don’t understand what they owe, why they owe it, and when payment is due, they are less likely to pay promptly.
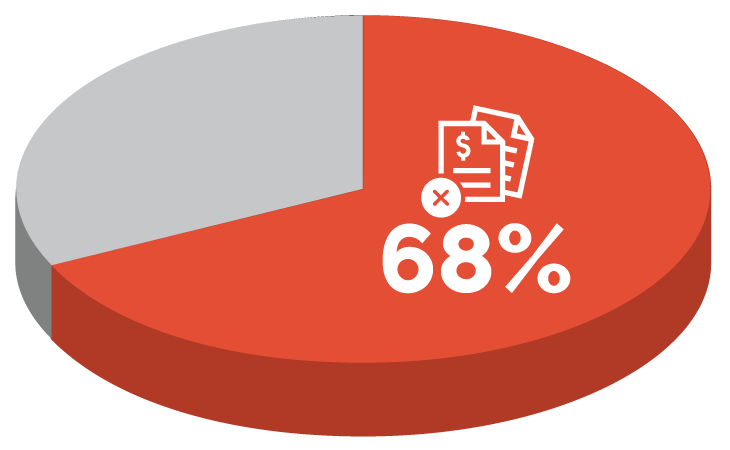
For example, a 2022 survey found that:
- 68% of adults with unpaid medical bills in the past five years reported that they did not pay the medical bill in full or only partially paid it because they thought their insurance was covering it.
- 44% of adults reported that they did not pay the medical bill in full or only partially paid it because they were not sure if the medical bill was accurate.
Such misunderstandings necessitate additional follow-up efforts from billing departments, including phone calls, mailed notices, and sometimes third-party collection interventions.
Additionally, poor communication can lead to a higher incidence of billing disputes and complaints. Addressing these disputes involves extensive staff time to review the case, communicate with insurance providers, and engage in lengthy discussions with the patient to clarify and rectify the situation. Such activities increase direct labor costs and divert staff from other revenue-generating activities, compounding the financial impact.
To mitigate these costs, healthcare organizations must prioritize clear and effective patient communication. Strategies might include:
- Enhanced upfront communication: Providing patients with clear, concise information about their estimated charges, insurance coverage, and out-of-pocket costs at the point of service.
- Transparent billing statements: Designing billing statements that are easy to understand, with itemized charges clearly linked to received services.
- Accessible patient support services: Offering readily accessible patient service lines or online portals where patients can get help with their billing questions and make payments encourages timely resolutions of billing issues and promotes timely payments.
5. Identify Opportunities to Outsource
Identifying opportunities to outsource certain functions in the healthcare revenue cycle can significantly reduce the cost-to-collect.
Outsourcing allows healthcare providers to leverage expertise and advanced technology from specialists who act as an extension of the current billing staff. Combining technology and reimbursement expertise results in faster cash collection and more efficient operations.
For example, we’ve helped our clients:
- Reduce 80% of aged receivables to >120 days within the first 6 months
- Increase revenue by 10% with automated coverage discovery
- Increase collections and denial efficiency by 30%
- See a 48% overall improvement in patient collections
Key benefits of outsourcing:
- Cost efficiency through specialization: Outsourcing transfers specific tasks to providers who specialize in those areas, using their expertise and optimized processes to execute tasks at a lower cost. This results in higher accuracy, fewer denials, and faster payments, directly impacting the cost-to-collect.
- Reduction in labor costs: Outsourcing can significantly reduce labor costs associated with hiring, training, and maintaining an in-house team for non-core functions. It transforms fixed labor costs into variable costs that scale with the volume of work, providing flexibility and reducing financial strain.
- Focus on core competencies: Outsourcing administrative tasks allows healthcare organizations to reallocate resources towards primary care services, improving patient care and operational efficiencies. This shift helps enhance the quality of patient services, which can drive revenue and improve patient satisfaction.
We’ve helped our clients:
Reducing cost-to-collect requires an expert and multifaceted approach. We help healthcare organizations improve their revenue cycle management through robust technology and expert knowledge—see how you could benefit via a free RCM assessment.