Did you know?
- 14 million people in the U.S. owe over $1,000 in medical debt, and about 3 million people owe more than $10,000 in medical debt.¹
- In 2022 and 2023, providers collected about $500.5 million for services rendered, less than half the amount owed.²
While growing medical debt and patients’ inability to pay service providers could stem from a plethora of external issues, one thing healthcare organizations can control is their billing processes and the experience they provide their patients.
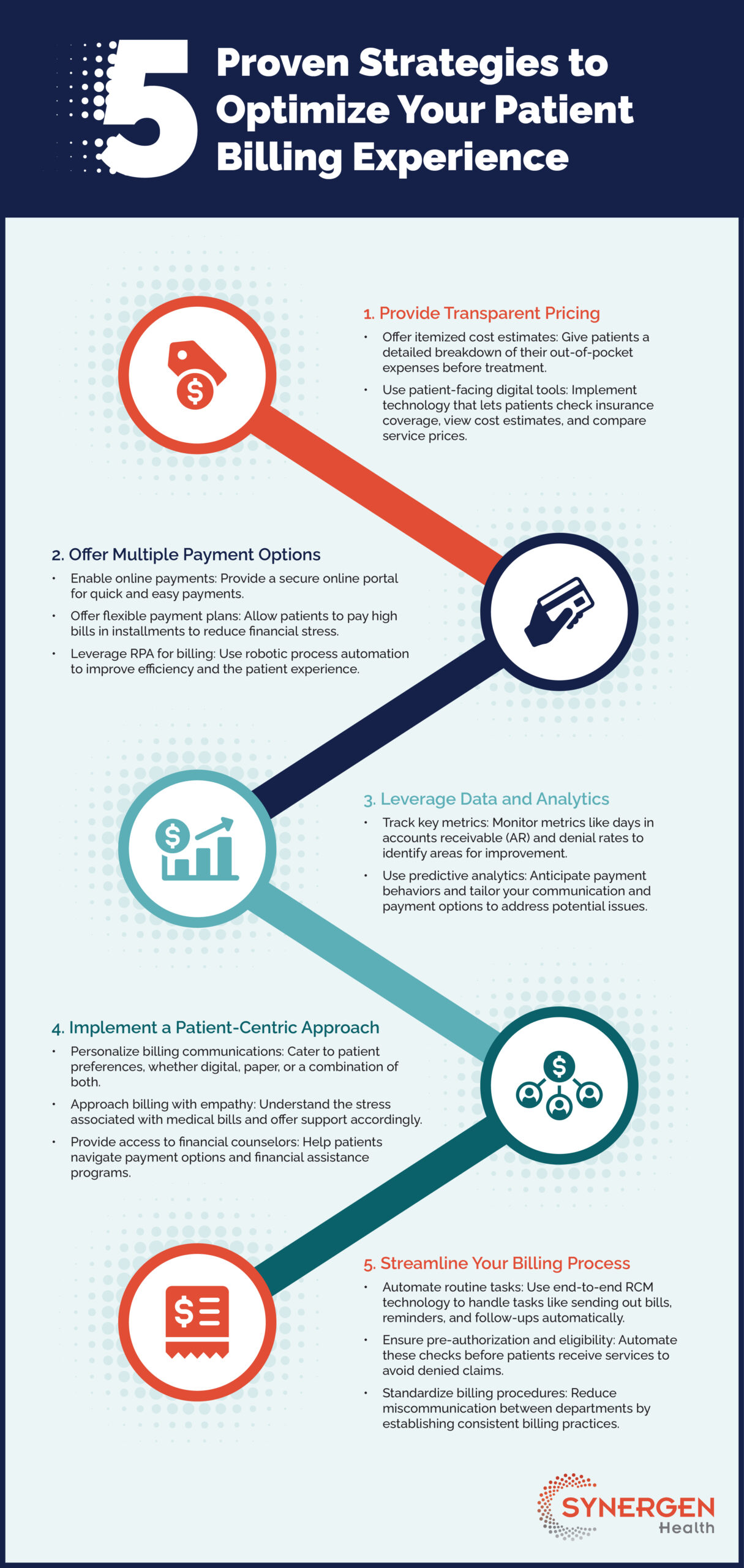
5 Proven Strategies to Optimize Your Patient Billing Experience
1. Provide Transparent Pricing
Offer itemized cost estimates: Give patients a detailed breakdown of their out-of-pocket expenses before treatment.
Use patient-facing digital tools: Implement technology that lets patients check insurance coverage, view cost estimates, and compare service prices.
2. Offer Multiple Payment Options
Enable online payments: Provide a secure online portal for quick and easy payments.
Offer flexible payment plans: Allow patients to pay high bills in installments to reduce financial stress.
Leverage RPA for billing: Use robotic process automation to improve efficiency and the patient experience.
3. Leverage Data and Analytics
Track key metrics: Monitor metrics like days in accounts receivable (AR) and denial rates to identify areas for improvement.
Use predictive analytics: Anticipate payment behaviors and tailor your communication and payment options to address potential issues.
4. Implement a Patient-Centric Approach
Personalize billing communications: Cater to patient preferences, whether digital, paper, or a combination of both.
Approach billing with empathy: Understand the stress associated with medical bills and offer support accordingly.
Provide access to financial counselors: Help patients navigate payment options and financial assistance programs.
5. Streamline Your Billing Process
Automate routine tasks: Use end-to-end RCM technology to handle tasks like sending out bills, reminders, and follow-ups automatically.
Ensure pre-authorization and eligibility: Automate these checks before patients receive services to avoid denied claims.
Standardize billing procedures: Reduce miscommunication between departments by establishing consistent billing practices.