Amid a global challenge of staff shortages in healthcare, the impact on revenue cycle management (RCM) is not often discussed, but significant nonetheless.
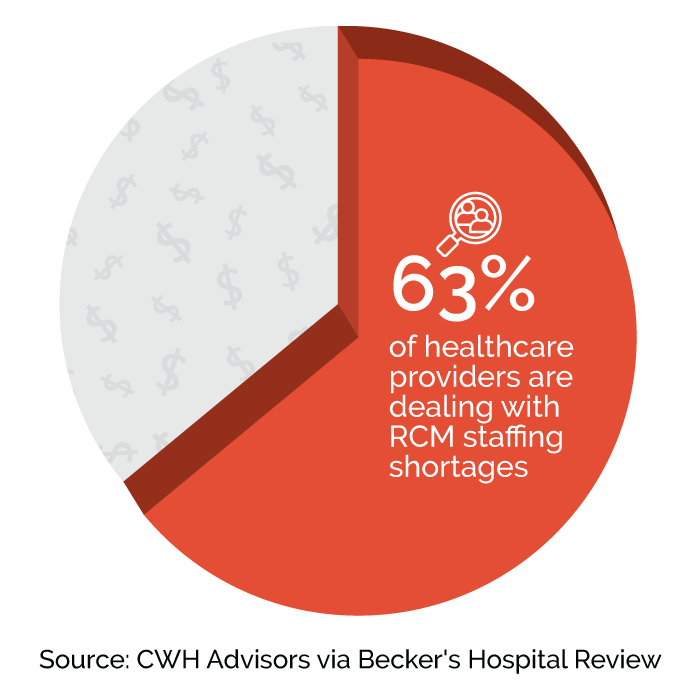
With 63% of providers grappling with RCM staff shortages, the need for a comprehensive solution is more critical than ever.
Innovative technological solutions can mitigate the effects of staff shortages on RCM and upskill current team members, ensuring healthcare organizations can maintain their financial health and continue to provide high-quality care.
The Challenge of Staff Shortages in RCM
RCM is the backbone of healthcare operations, playing a pivotal role in maintaining the financial health of healthcare providers.
However, staff shortages, exacerbated by the COVID-19 pandemic and other factors, have severely impacted RCM processes. These shortages affect billing, coding, and patient financial services, leading to delays in billing, increased errors, and a negative impact on cash flow. Claim denials put healthcare organizations in a constant state of catchup as the caseload can pile up endlessly.
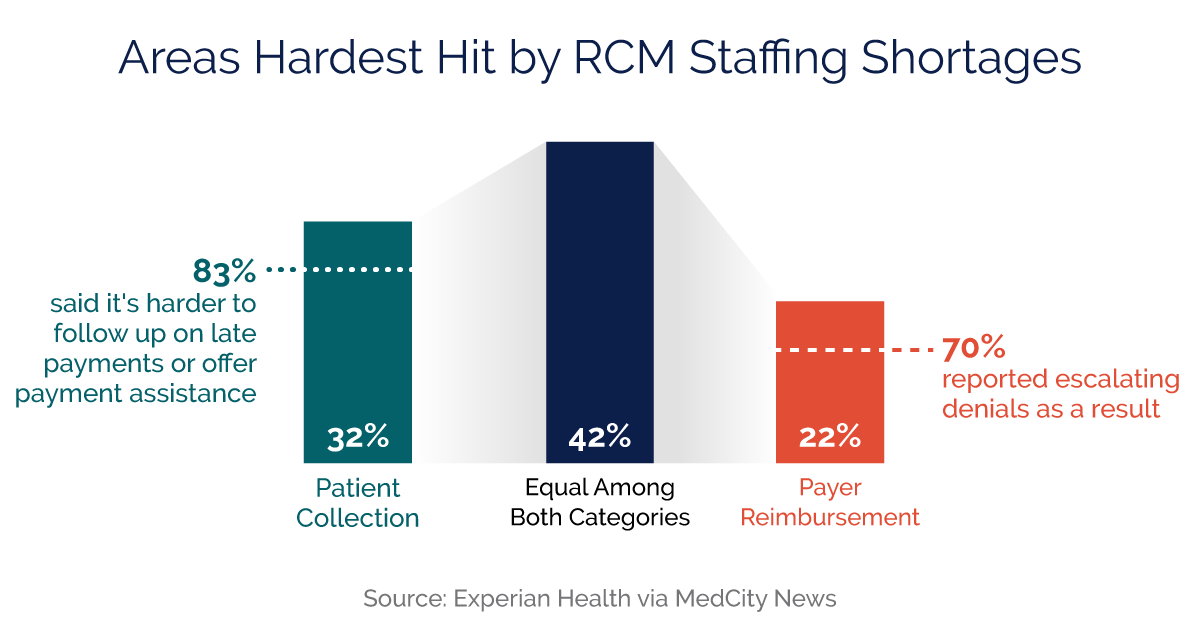
A recent Experian Health survey revealed that 32% of respondents found patient collection to be the hardest hit area, versus 22% for payer reimbursement, with 42% stating the impact is equal among both categories. Certainly, this presents a challenge, but also an opportunity to upskill the current workforce if automation is allowed to catch errors that human coders often do not.
Leveraging the Right Technology
Technology-driven, end-to-end solutions that leverage automation, AI, and an experienced client management team can overcome the most daunting of staffing challenges.
Automation and AI can streamline RCM processes, reduce errors, and alleviate the workload on existing staff. Partnering with a qualified vendor for critical RCM functions allows healthcare providers to focus on what they do best: patient care.
RCM professionals should seek expertise in providing tailor-made, specialty-specific RCM solutions that adapt to the unique needs of healthcare providers, ensuring that each organization can overcome its specific hurdles and roadblocks.
2.3
2.3M monthly manual tasks automated
450
450 FTEs saved with automation
21
21+ billing platforms integrated
900
900+ software engineers, consultants, and analysts
1
1 dedicated account team
Revenue Cycle Success Stories
An end-to-end RCM vendor’s impact is best illustrated through its real-life success stories.
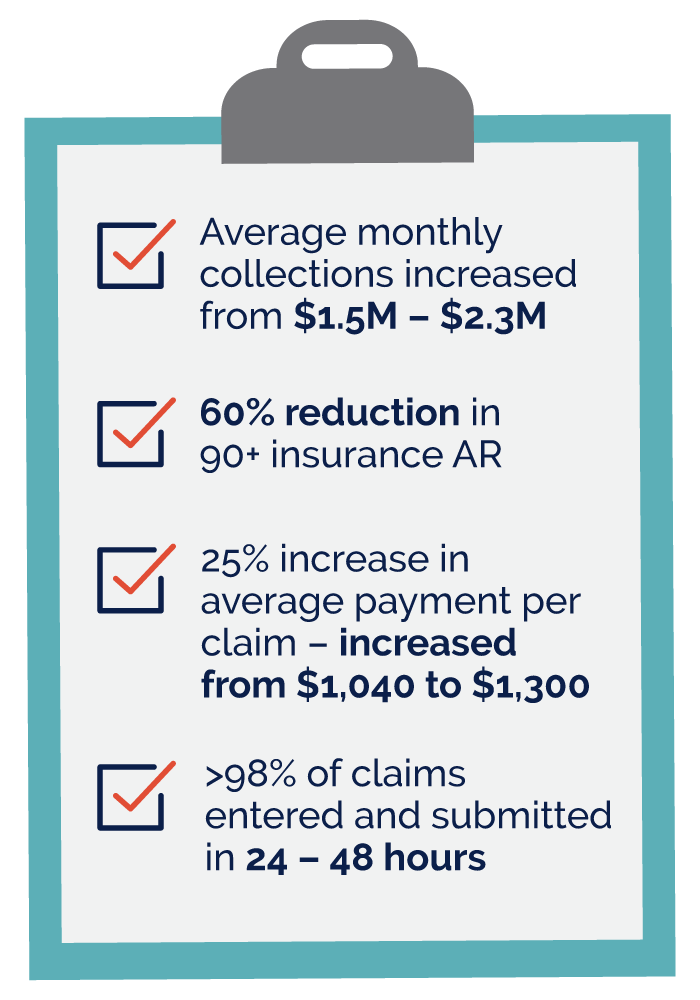
For instance, CityDoc utilized end-to-end RCM solutions to mitigate staff shortages, thereby improving financial outcomes.
- 90+ AR reduced by 95% from $111K in 2014 to $6K at present
- Average revenue/claim increased by 11% (from $133–$148)
- >95% of claims submitted within 24 hours from DOS
- First-time payment rate of 98%
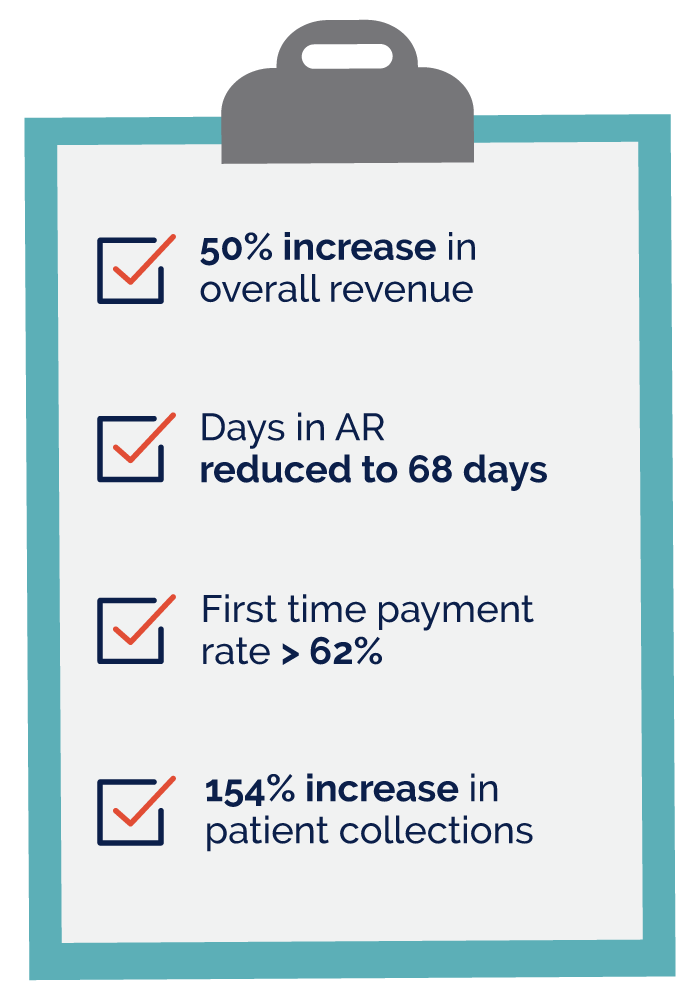
Berenson Cancer Center had faced challenges related to transparency in its RCM processes and poor customer service. The organization stepped in the right direction with a no-cost, no-obligation benchmarking assessment of its RCM operations.
- 100% transparency into RCM processes
- 3% increase in reimbursement ratio after transitioning to SGH
- First-time payment rates improved to 98–99%
Implementation and Onboarding Process
Transitioning to an end-to-end RCM platform is designed to be seamless, ensuring ease of integration with existing systems. The process involves detailed steps to adapt the vendor’s solutions to the healthcare provider’s specific needs, supported by comprehensive onboarding assistance.
The ongoing support and optimization services offered by SYNERGEN Health ensure that healthcare organizations continue to improve their RCM processes and overall financial health.
New Solutions for Growing Challenges
Addressing staff shortages in RCM is imperative for the financial health of healthcare organizations.
SYNERGEN Health provides a robust solution through technology-driven strategies and client management options, ensuring healthcare providers can navigate these challenges effectively. By exploring our offerings, healthcare organizations can take proactive steps toward enhancing their RCM processes, ultimately leading to improved financial outcomes, efficiency, and patient satisfaction.
To discover how SYNERGEN Health can transform your RCM processes, request your opportunity assessment today.